Introduction: The recent ICC introduced a novel category denominated “myeloid neoplasms with mutated TP53” (MN- TP53) that includes: 1) myelodysplastic syndromes (MDS- TP53) in cases with multi-hit TP53 or mutated TP53 with complex karyotype, and blasts <10%; 2) MDS/acute myeloid leukemia (MDS/AML- TP53) in those with TP53 mutations and blasts between 10-19% and 3) AML- TP53 in patients with TP53 mutations and blasts ≥ 20%. In all the aforementioned groups, a variant allele frequency (VAF) >10% of TP53 gene is required for inclusion. As opposite to ICC, the WHO 2022 classification does not recognize this mutated group as a distinct entity, maintaining the 20% blast count as the boundary between MDS and AML, with no intermediate category. The objective of this study was to assess, in a multicentric series, whether the 10% blast cutoff has clinical implications in the MN- TP53 category.
Methods: All patients diagnosed with MDS and AML with MN- TP53 criteria according to ICC between 2009-2023 were included from four Spanish centers. TP53 gene status was assessed by Next-Generation Sequencing.
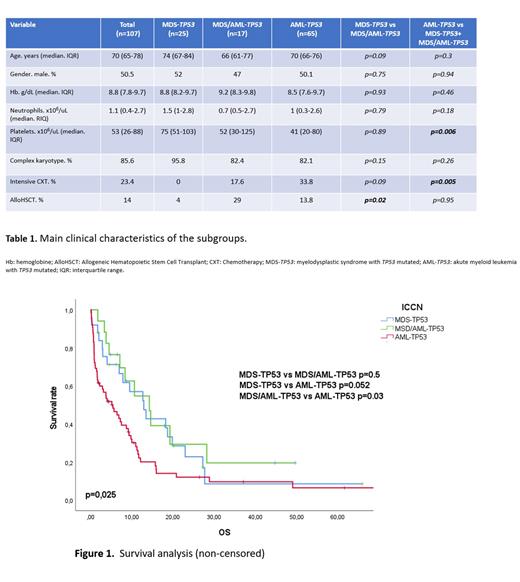
Results: A total of 107 patients were included: 25 (23.4%) MDS- TP53, 17 (15.9%) MDS/AML- TP53, and 65 (60.7%) AML- TP53. The median age at diagnosis was 70 years (interquartile range, IQR: 65-78) and 54 (50.5%) were male. Among all patients, 83 (77.6%) presented a complex karyotype. After a median follow-up of 6.2 months, 84 patients (78.5%) died, resulting in a median overall survival (OS) of 7.9 months.
The median OS for the MDS- TP53, MDS/AML- TP53 and AML- TP53 groups was 12.9, 14.3 and 5.4 months, respectively (p=0.025) (Figure 1). Paired comparisons showed similar OS between MDS- TP53 and MDS/AML- TP53 groups (p=0.5) but shorter OS in AML- TP53 group when confronted with MDS/AML- TP53 (p=0.03) or AML- TP53 with MDS- TP53 (p=0.052).
In addition to potential outcome dissimilarities, clinical characteristics at baseline were also compared (Table 1). Again, there were no differences between the MDS- TP53 and MDS/AML- TP53 groups at diagnosis. Intensity of chemotherapy treatment and frequency of allogenic hematopoietic stem cell transplant (alloHSCT) were also analyzed. One important difference between MDS- TP53 and MDS/AML- TP53 was that 4% and 29% of cases underwent alloHSCT, respectively. To assess the potential impact of allotransplant in this cohort, the survival analysis was repeated censoring the OS at the infusion date. The OS between groups MDS- TP53 and MDS/AML remained comparable (p=0,98).
Conclusions: In our cohort, patients with MDS- TP53 and MDS/AML- TP53 exhibit similar clinical behavior, in contrast to AML- TP53, suggesting that the newly proposed 10% blasts cutoff is not adding clinical value to the management of these entities.
Disclosures
Tormo:AbbVie: Honoraria; Pfizer: Honoraria; MSD: Honoraria; BMS: Honoraria; Astellas: Honoraria. Salamero:Pfizer: Consultancy, Honoraria; Jazz: Consultancy, Honoraria; BMS: Consultancy, Honoraria; Astellas: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria. Tazon:Bristol Myer Squibb: Honoraria. Bosch:Novartis: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; Mundipharma: Consultancy, Honoraria; Lilly: Consultancy; Roche: Honoraria; BeiGene: Consultancy; AstraZeneca: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Karyospharm: Other; Celgene: Consultancy, Honoraria; Roche: Consultancy, Honoraria. Jerez:GILEAD: Research Funding; Astrazeneca: Research Funding; Novartis: Consultancy; BMS: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal